CASE OF THE QUARTER
October-December 2020
A previously-healthy, normal-weight 70-year-old female without osteoporosis, presents with the following:
- 3/2019 Sudden pain with weight-bearing in the right hip/groin, stiffness, radiculopathy. Conservative physical therapy initiated.
- 7/2019: Continued pain, requires a cane to ambulate. Radiograph mild degenerative joint disease/osteoarthritis. Cortisone injection into SI joint provides relief; no injections given to right hip joint.
- 10/2019: Pain continues. Retrospective review of this late MRI reveals the final diagnosis that caused the degenerative joint disease/osteoarthritis (DJD/OA), now moderate to severe. A total right hip arthroplasty is performed, ten months later, 5/2020, due to COVID-19.
The surgeon thought and submitted this case to pathology as common DJD/OA.
QUIZ
1. What is your diagnosis?
A. Primary osteonecrosis.
B. Primary osteoarthritis.
C. Subchondral enchondroma.
D. Subchondral insufficiency fracture.
E. Primary osteomalacia.
2. What are the known risk factors for subchondral insufficiency fracture (SIF)?
A. Steroids or alcohol abuse
B. Trauma – high external force
C. Bisphosphonate fracture
D. Obesity, osteoporosis, elder female
E. Osteomyelitis
3. Which one of the following is correct?
A. Subchondral insufficiency fracture cannot be treated by rest.
B. Subchondral insufficiency fracture is typically bilateral and due to steroids.
C. Subchondral insufficiency fracture occurs due to abnormal activity (strong force) on normal bone.
D. Subchondral insufficiency fracture occurs in obese with weight bearing, may be elderly female with osteoporosis.
E. Subchondral insufficiency fracture occurs with high energy force trauma to osteoporotic bone.
Quiz Answers
1. D
2. D
3. D
Question 1 Discussion
Correct Answer: D
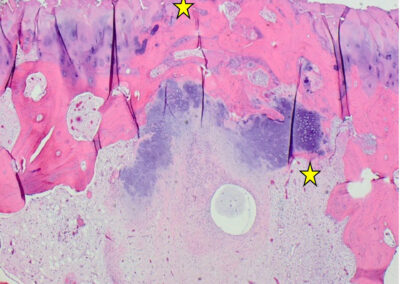
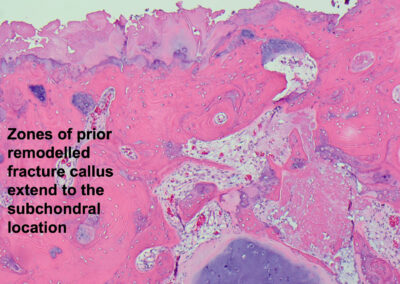
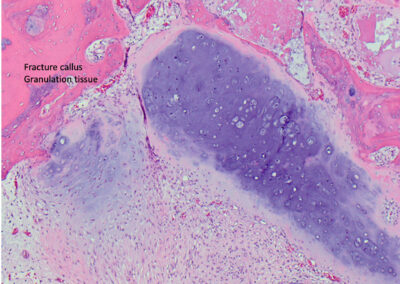
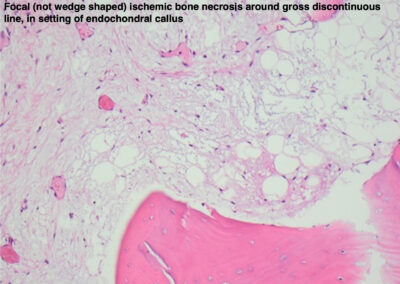
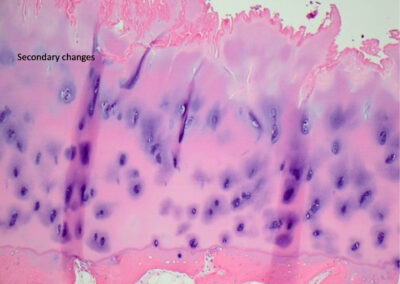
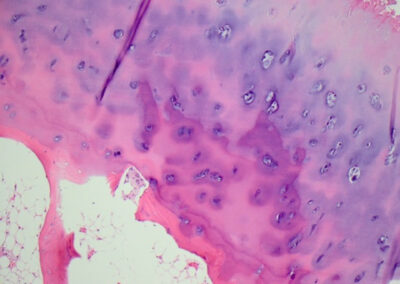
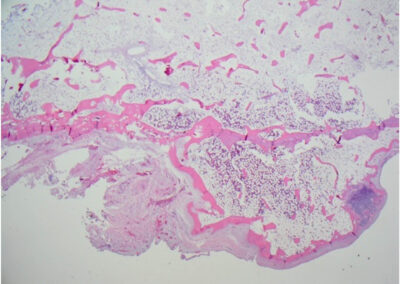
(The correct diagnosis is subchondral insufficiency fracture (SIF) with secondary degenerative joint disease/osteoarthritis (DJD/OA) and possible foci of ischemic necrosis only around the discontinuous fracture line. SIF was first described as an entity by Yamamoto and Bullough (2000) as a type of stress fracture due to bone fragility, poor mineralization, impaired elastic resistance, normal force on weakened bone, often in the femoral head and can also occur in the knee and shoulder. This came to pathology as ordinary DJD/OA without looking at the history of 1) sudden pain, 2) gross serpiginous line with white around it, 3) microscopic fracture callus that extends to articular surface, no large areas of osteonecrosis/avascular necrosis, marked secondary DJD/OA. The risk factors for SIF include obesity, older age, female, transient osteoporosis, and weight bearing/normal activity. The patient did not have imaging immediately and continued to walk on a subchondral fracture, causing rapidly-progressive DJD/OA. The radiograph suggested only mild OA and did not account for patient’s sudden, drastic pain. Re-review of a late MRI did finally demonstrate SIF, too late for conservative management to prevent severe DJD/OA and arthroplasty. The gross pathology reveals whitish (microscopically ischemic) areas around a serpiginous, discontinuous convex fracture line with secondary severe DJD/OA. Microscopic demonstrates endochondral callus that extends subchondral, granulation tissue, focal areas of ischemic necrosis (not large wedge of osteonecrosis) and changes of secondary DJD/OA, including cloning, reduplication of tidemark, fibrillation, osteophyte. While there are focally thin trabecula, this patient was not found radiologically to have osteoporosis. If this were caught early, the treatment is conservative with rest, bisphosphonates, and even RANK-L inhibitors including Denosumab. Even though there is consideration that SIF fracture has clinicopathologic and radiologic overlap with primary osteonecrosis (ON), these are two separate entities and are treated differently. SIF typically occurs in obese patients with normal weight bearing and sudden onset of pain and is convex on imaging with a discontinuous serpiginous fracture line, whereas ON occurs with steroid or alcohol abuse or other and may be bilateral, younger patient, pain worsens over time, and is concave on imaging, wedge-shaped necrosis surrounded by hyperemia. This distinction is made on the basis of the depth of the abnormality, a usually wedge shape macroscopically and microscopically and particularly on the basis of necrosis of bone which represents a generous zone of original non remodelled mature lamellar host cancellous bone. This contrasts with the secondary ischemic necrosis or osteonecrosis in DJD/OA which is composed of sclerotic admixture of woven and lamellar bone).


Feedback
A. Not Correct. (There is secondary focal grossly white and microscopically ischemic necrosis around the area of thin serpiginous, discontinuous line, but not wedge-shaped of primary osteonecrosis. Even though there is consideration that SIF fracture has clinicopathologic and radiologic overlap with primary osteonecrosis (ON), these are two separate entities and are treated differently. SIF typically occurs in obese patients with normal weight bearing and sudden onset of pain and is convex on imaging with a discontinuous serpiginous fracture line, whereas ON occurs with steroid or alcohol abuse or other and may be bilateral, younger patient, pain worsens over time, and is concave on imaging, wedge-shaped necrosis surrounded by hyperemia.
B. Not Correct. (There is secondary osteoarthritis that progresses and requires arthroplasty; this is secondary to the process identified on MRI, only mild OA was radiologically present at the sudden onset of patient’s pain; radiologic confirmation of other entity is the final diagnosis)
C. Not Correct. (The cartilage is part of endochondral ossification and is not neoplastic)
E. Not Correct. (Characteristic systemic radiologic, specific laboratory, or microscopic osteoclastic tunneling or increased seams of unmineralized bone features are not present.)

Question 2 Discussion
Correct Answer: D
(Risk factors for SIF include obesity, transient or constant osteoporosis, female, normal ambulation, ie. normal ambulation/activity weight bearing on weakened bone or the amount or quality of bone is insufficient for the amount of weight the bone has to bear.)

Feedback
A. This is incorrect. (Steroids and alcohol abuse are a risk factor for osteonecrosis, which can be bilateral and in younger people).
C. This is incorrect. (Bisphosphonate fracture occurs in a small percentage of patients treated with bisphosphonate–transverse fractures of long bones, by “freezing” the skeleton – lack of remodeling allows for weakening of the bone and microcrack accumulation)
E. This is incorrect. (Osteomyelitis is not a risk factor for subchondral insufficiency fracture; one would observe neutrophils with acute and plasma cells, fibrosis and bone remodeling with chronic osteomyelitis, direct spread in diabetic often neuropathic adults, hematogenous spread in children).
Question 3 Discussion
Correct Answer: D
(Subchondral insufficiency fracture occurs in obese with weight bearing, may be elderly female with transient osteoporosis is the CORRECT answer)
Feedback
A. This is incorrect. (If SIF is properly diagnosed, often requires a) history of acute and constant pain and b) MRI for diagnosis, then rest can heal. If so, progression to secondary osteoarthritis and need for arthroplasty may be avoided)
B. This is incorrect. (Primary osteonecrosis, wedge shaped due to arcuate metaphyseal feeder vessel, may be bilateral and due to steroid use or alcohol or other)
C. This is incorrect. (SIF occurs with normal (weight-bearing) ambulation on top of weakened bone often with obesity, and may be with transient osteoporosis in elderly females)
E. This is incorrect. (SIF occurs with normal ambulation on top of weakened bone with obesity, and may be with transient osteoporosis in elderly females)
Why this is a great case
Subchondral insufficiency fracture (SIF) is an entity that is not well-known to pathologists.
In this case, SIF was extremely subtle and picked up by an astute musculoskeletal radiologist and upon review of gross and microscopic at the time of arthroplasty for “severe osteoarthritis”.
If the clinician recognized the sudden onset of pain and an MRI was performed sooner, recognition of an underlying subchondral insufficiency fracture by clinicoradiologic findings could lead to correct conservative treatment and might avoid progression to secondary severe osteoarthritis that required surgery for arthroplasty.
An MRI is the best modality for observing the subtle convex discontinuous serpiginous fracture line. These can be missed on radiograph; sometimes radiology is not performed immediately in patients with pain and they get “conservative” management. Injection of steroid into the SI joint did not treat the right hip subchondral insufficiency fracture (SIF).
This case emphasizes the value of a good gross description. Sometimes these subchondral fractures are eccentric in distribution and it is important to emphasise serial sectioning in order to identify the fracture which may be off center. Indeed the osteoarthritis may be the only abnormality visible to the pathologist if a single central section only is taken. The gross was performed by PA and residents and retrospective review after microscopic slide review and re-review of the MRI, the subchondral insufficiency fracture was appreciated. The clinical consideration was DJD/OA only.
The histopathologic changes illustrated in this case do express how challenging this diagnosis can be because the characteristic early fracture line with reactive bony callus forming a scaffold between pre-existing host trabeculae have essentially been entirely remodelled and now there is new organising woven and lamellar bone with a fibrous stroma and fibrocartilaginous callus associated with adjacent secondary osteoarthritis.
As a pathologist, it is best to be aware of this entity and look for this on the gross pathology submitted for “osteoarthritis” or “avascular necrosis”: 1) not confuse it with primary degenerative joint disease/osteoarthritis since there is an underlying cause or 2) due to focal white changes that represent focal (only) microscopic ischemic necrosis around the fracture callus —not confuse it with an alternate process of primary osteonecrosis or other.
Although there are specific risk factors for SIF, people who are otherwise healthy can have subchondral compression (stress) fractures without prior osteopenia with repeated normal ambulation.
This patient should not have been ambulating with SIF.
References
An VV, Broek MVD, Oussedik S. Subchondral Insufficiency Fracture in the Lateral Compartment of the Knee in a 64-Year-Old Marathon Runner. Knee Surg Relat Res. 2017;29(4):325-328. doi:10.5792/ksrr.17.049
“Board Style Review Questions.” PathologyOutlines.com. 2002-2020. Accessed at https://www.pathologyoutlines.com/review-questions?chid=55 Ghate SD, Samant A. Subchondral Insufficiency Fracture of Femoral head: Uncommon cause of Hip pain in Elderly. J Orthop Case Rep. 2012;2(2):7-9.
Ikemura A, Yamamoto T, Motomura G, Nakashima Y, Mawatari T, Iwamoto Y, The utility of clinical features for distinguishing subchondral insufficiency Fracture from osteonecrosis of the femoral head. Archives of Orthopedic Trauma Surgery. 2013; 133:1623-1627.
McClung, M. Role of RANKL inhibition in osteoporosis. Arthritis Res Ther 9, S3 (2007). https://doi.org/10.1186/ar2167
Yamamoto, T., Schneider, R. & Bullough, P. Subchondral insufficiency fracture of the femoral head: histopathologic correlation with MRI. Skeletal Radiol 30, 247–254 (2001). https://doi.org/10.1007/s002560100348
Yamamoto, T. Subchondral Insufficiency Fracture of the Femoral Head. Clinics in Orthapedic Surgery. 2012;4 173-180. Accessed 6/11/20 https://doi.org/10.4055/cios.2012.4.3.173 Yamamoto T, Iwamoto Y, Schneider R, et al. Histopathological prevalence of subchondral insufficiency fracture of the femoral head. Annals of the Rheumatic Diseases 2008;67:150-153.
Author(s)
Brandon Williams
Donald J. Flemming
Julie C. Fanburg-Smith
Penn State College of Medicine and Departments of Pathology, Pediatrics, Orthpaedics, Radiology
Penn State Health, MS Hershey Medical Center
Hershey, PA 17033